Healing middle ear lesions with Thymosin β4
In a recent study, researchers explored the use of Thymosin β4 (Tβ4) to promote healing in tympanic membrane perforations. They found that Tβ4 affected the behavior of epidermal and epithelial cells in the tympanic membrane and may be useful in promoting cell migration and proliferation to aid healing.
Hearing loss affects over 1.5 billion people worldwide, and it can have a significant impact on quality of life. Whether caused by genetic factors, infection, age-related degeneration, or injury, hearing loss can lead to social isolation, frustration, and even unemployment. In fact, the World Health Organization estimates that unaddressed hearing loss costs the global economy $750 billion each year.
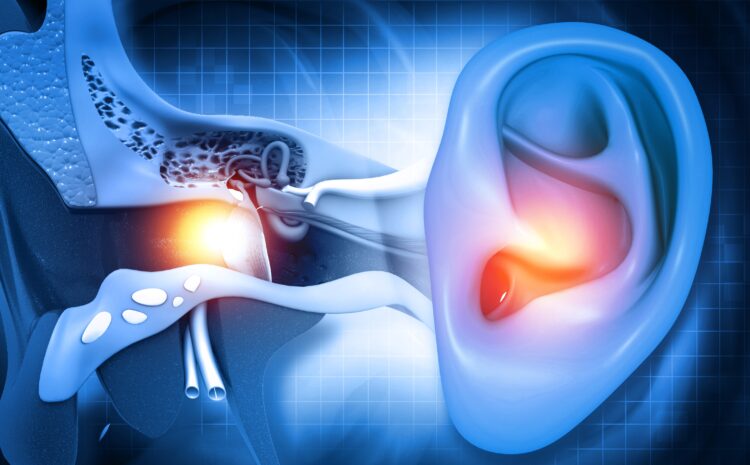
There are two main types of hearing loss: sensorineural and conductive. Sensorineural hearing loss occurs when there is damage to the inner ear or auditory pathway, while conductive hearing loss is caused by problems in the outer or middle ear that affect sound conduction and amplification.
The tympanic membrane, also known as the eardrum, is a cone-shaped organ located between the external auditory canal and the tympanic cavity. Its inferior part, the pars tensa, is fixed to the tympanic bone through the fibrocartilaginous annulus, whereas the malleus is attached to the bone with the malleolar ligaments forming the anterior and posterior malleolar folds on the surface of the tympanic membrane. The malleolar folds separate the superior part, the pars flaccida, from the pars tensa. Histologically, the tympanic membrane consists of three layers: the outer surface contains the stratified squamous keratinized epithelium, which is continuous with the epithelium of the external auditory canal; the inner surface is covered by simple cuboidal epithelium, and the middle layer is made of fibroblastic connective tissue, containing the vessels and nerves that supply the membrane.
Tympanic membrane perforation primarily occurs due to injury or inflammation, which can be a result of acute otitis media or granular myringitis. While 80-94% of all acute perforations spontaneously heal within three months, the remaining cases become inveterate, resulting in a chronic suppurative otitis media. In addition to conductive hearing loss due to perforation and consequential insufficient amplification of the tympanic membrane, chronic suppurative otitis media limits the patient’s quality of life, especially when participating in aquatic activities or bathing. Moreover, severe complications such as deafness, dizziness, meningitis, or brain abscess may also occur. Clinically, chronic suppurative otitis media primarily requires surgical intervention.
Currently, there are several technologies and materials available that may be utilized for the reconstruction of the tympanic membrane. Autologous grafts such as the temporal fascia, perichondrium, cartilage, or lobulus fat are commonly employed tissue types and result in a closure rate of 71-97%. Additional materials such as paper, silk, chitosan, collagen, polydimethyl siloxane, or even acellular dermis as an allograft effectively serve in mending reconstruction. Recently, the utilization of various bioactive molecules, such as basic fibroblast growth factor or epidermal growth factor, emerged as promising means to stimulate and heal tympanic membrane perforations in various species, including humans.
However, despite these treatments, healing of tympanic membrane perforations remains insufficient, and there is a need for substances that can actively promote cell migration and proliferation in the middle ear. That’s where Thymosin β4 comes in.
Tβ4 possesses many regenerative properties in various organ systems. Researchers recently conducted a study to investigate the impact of externally administered Tβ4 on the middle ear, specifically the tympanic membrane.
The researchers harvested tympanic membranes from adult mice and treated them with Tβ4 or a placebo solution. They then measured cell migration and proliferation and performed immunocytochemical analyses to determine the nature of the targeted molecules.
The results of the study were promising. The researchers found that Tβ4 affects the behavior of epidermal and epithelial cells of the tympanic membrane in vitro, and that it likely targets local epidermal progenitor cells. This suggests that Tβ4 could be used clinically to promote healing of tympanic membrane perforations.
While further research is needed to confirm these findings and determine the optimal dosage and method of administration, the potential benefits of Tβ4 in promoting healing of tympanic membrane perforations are clear. This could lead to improved quality of life for millions of people worldwide who suffer from conductive hearing loss.
In the meantime, it’s important for individuals to take steps to protect their hearing. This includes avoiding exposure to loud noises, wearing ear protection when necessary, and seeking medical attention if hearing loss is suspected. With continued research and advances in treatment, we can hope to reduce the impact of hearing loss on individuals and society as a whole.
Full article can be found here: https://doi.org/10.1016/j.intimp.2023.109830
